The Cost of Breathing: Why Respiratory Drugs Remain in the NHS Top 10
Breathing is something most of us take for granted – until we can’t. In 2025, respiratory diseases like asthma and chronic obstructive pulmonary disease (COPD) continue to affect millions across the UK. Helping people breathe better doesn’t come cheap. In fact, respiratory medications remain among the top 10 drugs the NHS spends the most money on – both in terms of how often they’re prescribed and how much they cost.
This article breaks down why these drugs are so commonly used, what drives their costs, and how the NHS is trying to manage this growing demand.
Why Are Respiratory Drugs So Common?
Conditions like asthma and COPD are chronic, meaning they last a long time – often a lifetime. These diseases cause tightening of the airways, making it difficult to breathe, especially during flare-ups or in response to triggers like pollution, cold air, or allergens.
To help manage these conditions, millions of people use inhalers every day. These devices deliver medication straight into the lungs to:
- Prevent symptoms from occurring (maintenance treatment)
- Provide relief during sudden breathing difficulties (rescue treatment)
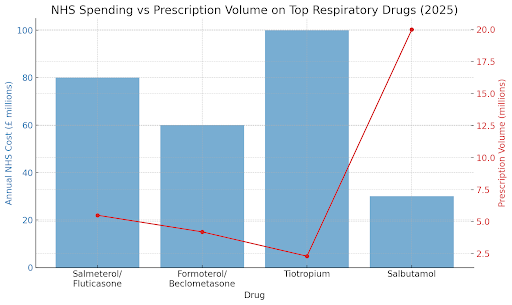
Common drugs used in inhalers include:
- Salmeterol/fluticasone (e.g. Seretide)
- Formoterol/beclometasone
- Tiotropium
- Salbutamol (commonly known as the "blue inhaler")
Who Needs These Medications?
The scale of respiratory illness in the UK is huge:
- Around 12 million people are currently receiving treatment for asthma, COPD, or other lung conditions3.
- Asthma alone causes over 60,000 hospital admissions and more than 1,000 deaths each year4.
To avoid these outcomes, people need to stay on their medications consistently, sometimes using multiple inhalers each day. That quickly adds up.
The NHS’s Respiratory Bill: What’s Driving the Cost?
Even though many inhalers are now available as generics (lower-cost versions of brand-name drugs), the cost of treating respiratory disease is still very high. Here's why:
1. Inhalers Are Used Every Day, Often for Life
Respiratory diseases aren’t like infections that clear up after a week of antibiotics. They require daily treatment – often for years or decades. That means patients may use hundreds of inhalers over a lifetime, sometimes two or more different types at once.
2. Combination Inhalers Are Expensive
Inhalers that combine multiple medicines (like an inhaled steroid and a long-acting bronchodilator) are commonly used to improve control. These combination treatments – like Seretide (salmeterol/fluticasone) – can cost significantly more per unit than simpler inhalers2.
3. High Prescription Volume
Even cheap drugs like salbutamol (the blue "rescue" inhaler) become costly when prescribed millions of times per year. In fact, salbutamol remains one of the top five most prescribed drugs in the NHS, simply due to how often it's used5.
4. Newer Drugs and Devices
Drugs like tiotropium, a long-acting bronchodilator used in COPD, are still costly, especially when delivered in newer inhaler devices that are easier to use or more eco-friendly6. These new technologies often carry a premium price.
Environmental Costs: Inhalers and Carbon Emissions
There’s another important factor many people overlook: the environmental impact of inhalers.
Some inhalers, especially pressurised metered-dose inhalers (pMDIs), use hydrofluorocarbons (HFCs) to deliver the drug. These gases are potent greenhouse gases, contributing to NHS carbon emissions7.
In fact, inhalers account for about 3% of the NHS’s total carbon footprint. To address this, current guidelines recommend switching patients – when appropriate – to dry powder inhalers (DPIs), which are much better for the environment8.
Smart Inhalers: A High-Tech Solution?
Another growing trend in 2025 is the rise of “smart inhalers.” These are inhalers that include sensors to track how often and how well a patient is using them. They can send reminders or alerts to both the patient and their healthcare team.
Smart inhalers offer big potential benefits:
- Better adherence to treatment (fewer missed doses)
- Fewer asthma attacks
- Less need for hospital care
However, they also come with higher upfront costs, and adoption across the NHS has been slow and uneven9.
Physiotherapists and Respiratory Care: A Team Effort
You might not immediately think of physiotherapists when it comes to breathing problems – but they play a key role, especially for people with COPD or severe asthma.
Physiotherapists can:
- Teach patients breathing exercises to improve lung capacity
- Help with chest clearance techniques to remove mucus
- Support pulmonary rehabilitation, a structured programme combining exercise and education
Several of our team at Surrey Physio are trained in breathing exercises and techniques. We also perform rib stretches, lung pumping, and train patients on diaphragmatic breathing, as well as other rib techniques. When patients are educated about what to do if breathing becomes restricted, they can keep calm and stay as relaxed as possible, to minimise further exacerbation.
And it really helps! We have had many patients improve with conditions ranging from asthma to long COVID. As medication costs rise, these non-drug interventions become even more valuable in helping people prevent flare ups.
What’s Next? Balancing Breath and Budget
With rising demand, environmental concerns, and a push for more personalised care, the NHS is trying to strike a balance between:
- Prescribing the right drugs
- Controlling costs
- Reducing emissions
- Improving patient outcomes
Future strategies may include:
- Encouraging eco-friendly inhaler switches
- Expanding the use of smart technologies
- Targeting better inhaler technique education (poor technique can waste medication and worsen symptoms)
- Promoting pulmonary rehab as a cost-effective complement to drug treatment
But ultimately, we should be deploying more physiotherapists to support patients with breathing education and respiration techniques to support good, effective breathing.
The Price of Helping People Breathe
In 2025, the NHS continues to invest heavily in respiratory drugs – not because it can afford to, but because it has to. Asthma and COPD remain major public health challenges, and inhaled medications are still the frontline defence against worsening symptoms, hospitalisation, and early death.
Whether it’s the daily use of salbutamol or the long-term cost of combination inhalers like Seretide, the NHS’s respiratory spending reflects both need and commitment. But as innovation, environmental pressures, and new care models emerge, the focus is shifting: from just spending more, to spending smarter.
References
- NHS Business Services Authority. Prescription Cost Analysis – England 2024/25. NHSBSA; 2025.
- OpenPrescribing.net. Top respiratory drugs by NHS expenditure.
- British Lung Foundation. The State of Lung Health in the UK. 2024.
- Asthma + Lung UK. Asthma facts and statistics.
- NHSBSA. Top 100 Prescribed Items by Volume – England 2025.
- NICE. Tiotropium for treating COPD. Technology Appraisal [TA232]; updated 2023.
- Wilkinson AJ et al. Costs and carbon footprint of inhalers used in the NHS. BMJ Open. 2019;9:e028763.
- NICE. Asthma: diagnosis, monitoring and chronic asthma management. Clinical Guideline [NG80]; updated 2024.
- Alshabani K et al. Smart inhalers in asthma and COPD: Current state and future directions. NPJ Digital Medicine. 2022;5(1):78.

